Reading Time: 4 minutes
Health centres in Bangladesh are overwhelmed with COVID-19 response. Many health facilities are refusing patients or closing down. Hospital beds are low in number, and many are being reserved for COVID-19 patients.
People from low-income households are facing the worst of the pandemic. Among them, pregnant women are being hit particularly hard. While most institutions and offices remain closed across the country, all 41 of BRAC’s maternity centres remain open to provide essential healthcare to pregnant and lactating women from low-income households.
BRAC’s maternity centres are part of the Manoshi project, established in 2007 to improve maternal, neonatal and child health status in Bangladesh’s urban slums. The centres offer low-cost, quality and culturally appropriate maternal and child health services to women living in slums.
Pregnant women come to the centres for check-ups, advice on pregnancy, and deliveries. The clinics are run by the midwives and medical officers, and doctors come in twice a week to meet patients with complications. A check-up performed by a midwife costs BDT 100 (USD 1.18) while delivery costs BDT 2,200 (USD 25.91). The cost of a check-up performed by a medical officer is BDT 150 (USD 1.76).
Read more: Facing COVID-19 with a disability
As cities are locked down due to COVID-19, medical officers and doctors are not always able to come to the centres. Midwives are rising to the challenge in these cases, keeping stringent health measures in place and consulting with doctors and medical officers through telephone.
Patients have to call in to book an appointment before visiting the centre. As part of safety precautions, midwives ask questions during those phone calls to identify whether the patient is showing symptoms of COVID-19. If the patient does not for example, have a fever or a dry cough, then they are given an appointment.
Patients are immediately made to wash their hands when they arrive in the centres. Their shoes and sandals are sprayed with disinfectant. They are met by midwives, who tend to them in personal protective wear. The clinics are sprayed with bleaching powder on a regular basis.
The Manoshi model
The Manoshi project uses two levels of trained female community health workers called shasthya shebika (health workers) and shasthya kormi (health volunteers) to reach the most vulnerable women in slums.
The health workers and volunteers make door-to-door visits to identify women of reproductive age and educate them on family planning. They also identify pregnant women and educate them on health and nutrition and basic antenatal check-up at home. Then, they bring in a medically-trained healthcare provider for a comprehensive antenatal check-up.
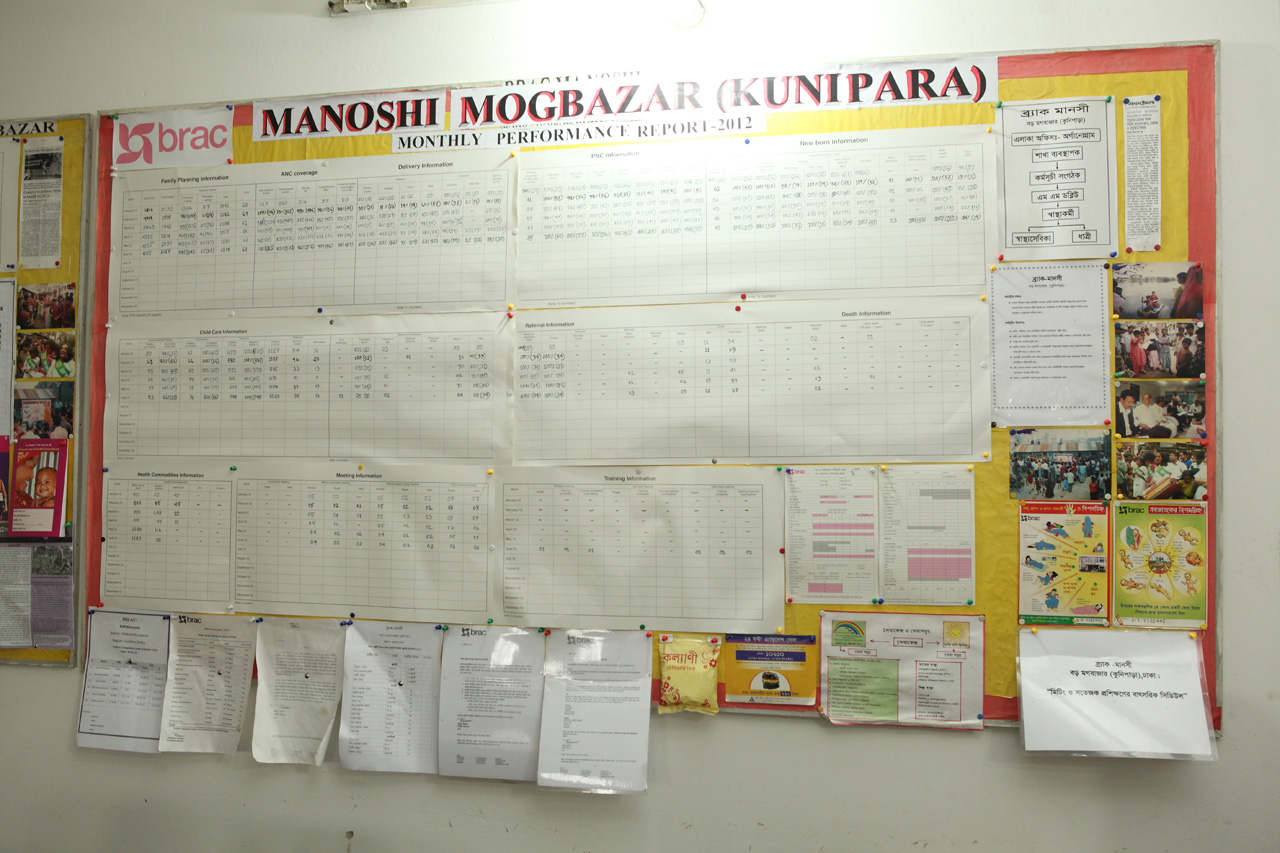
The maternity centers within the slums are designed to provide safe and dignified delivery services and facilitate timely referral to higher-level facilities in case of complications.
Manoshi is present in all major cities in Bangladesh, with a total population coverage of more than 7 million women living in slums. As the current lockdown has put a burden on hospitals and clinics, the importance of the services Manoshi’s midwives offer has magnified.
Providing essential care for expectant mothers
Fatema Akter works as a midwife, and has been with Manoshi for 10 years. She now shares her work with three other midwives in the maternity centres. In case of patients with serious cases, her team calls the medical officers for advice, who are providing telemedicine services.
When asked what challenges her patients are facing now, she said expectant mothers are scared.
“They worry about food, whether they can eat the things they normally eat. They are in fear of the virus, and when they are unsure if they can consume something, they call our numbers to confirm.”
Almost all patients’ biggest issue is money.
“People are out of work during this lockdown. Some women have to get a check-up, but do not have the money for it. Even if someone can afford it, they wonder if they will be able to afford the delivery fee when it will be time to go into labour”
“When a patient is unable to pay for a check-up, we are doing everything we can to ensure that they receive the care they need,” says Fatema.
Fatema lives 30 minutes away from the Manoshi centre in Dhaka’s Khilgaon area. She says it used to take longer for her to get to work, but the lockdown has made the roads eerily quiet.
“The centre feels different now. It’s quiet. Patients are still coming in, though not as many as before, but enough to keep us busy throughout the day. Since the shasthya shebika and shasthya kormi are not able to do routine home visits, they talk to their patients over the phone. If anyone needs care they tell them to come here.”
Why should maternity clinics remain open?
In a pandemic, the health sector is overburdened. The continuity of normal healthcare services is vital to curb fatalities from other diseases through this period.

The Ebola outbreaks in African countries serve as a grave reminder of what happens when resources are diverted to tackling one crisis, leaving another unattended. About 12,000 people died from the Ebola outbreak in 2014, but it was the closure of health facilities which resulted in many of the avoidable fatalities.
Ebola affected the health system severely. Pregnant women who did not receive treatment were lying unconscious outside of maternity centres, closed due to lockdown measures.
Measures must be in place to ensure this scenario does not replicate in Bangladesh. Even now, expectant mothers wonder whether hospitals themselves are safe and whether doctors are available. People from disadvantaged communities are usually the ones who face the brunt of the crisis.
When asked how she is experiencing coming to work during the lockdown, Fatema says, “I am fully aware that I need to practice utmost safety precautions at all times, wearing protective gear and taking all the safety measures. Protecting myself means protecting my family and my patients. I do not forget these precautions. I also do not forget the impact of our work – if our centre was closed, these women would not be able to receive the care they need. They would not know if their babies were healthy.”
Pregnancy is a medical emergency. Women not only need safe guidance through a pregnancy, they need to be tended to as soon as labour pains begin. Closed maternity centres not only leaves women behind in one of the most difficult times in their lives, it also increases the number of unskilled home deliveries, which will lead to an increased number of maternal and neonatal mortality.
Healthcare services such as maternity clinics must continue to ensure vulnerable patients can access services. Quality healthcare means that services are accessible to all, no matter what – especially during a deadly global pandemic.
Luba Khalili is Deputy Manager, BRAC Communications.





